Unless your kids have a gastrointestinal (GI) condition, you probably don’t spend a whole lot of time thinking about their colon or digestive tract. But for families of children who have GI diseases, it can greatly impact their daily lives.
This is one of the many reasons why I am part of a research team working to develop better models of the gastrointestinal tract, specifically the colon. Having a better model to study means a more accurate representation of the diseases occurring in the body, and hopefully more answers down the road.
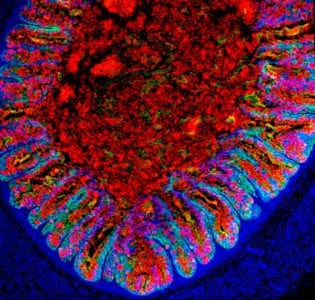
Recently, our research team took human pluripotent stem cells (the type of cells which can make copies of itself and can make any cell or tissue in the human body) and converted them into miniature colons. This was the first time that human colonic organoids have been successfully tissue-engineered in a lab. The findings were published in Cell Stem Cell.
We are excited about this research and the potential for it to help kids with gastrointestinal diseases. Here’s why:
5 REASONS TO BE EXCITED ABOUT SCIENTISTS GROWING HUMAN COLONS:
1. THE POTENTIAL FOR TRANSPLANTATION INTO PATIENTS.
Quite a few GI diseases could benefit from transplanting tissue-engineered colons back into patients’ bodies. For example, kids with necrotizing enterocolitis lose huge portions of their bowel, and essentially have short bowel syndrome for the rest of their lives. In theory, we could lengthen their colon via transplantation so that they wouldn’t have the issues associated with short bowel syndrome, like bile acid diarrhea. It’s difficult to project when the research will advance enough to begin doing this, but perhaps within a couple of decades.
2. THE POTENTIAL TO TEST THERAPEUTIC DRUGS.
Creating tissue-engineered colons could allow us to test the efficacy and toxicity of drugs before trying in humans. For instance, when patients have juvenile polyposis syndrome, they will develop polyps in the colon. Because of this, they will likely have their colon removed at some point in their life. If we modeled this disease in our tissue-engineered colon, we could look for drugs that might help to suppress the formation of polyps. And if we could prevent that from happening, we might be able to thwart both colon cancer and the removal of the colon in these patients. We think testing for therapeutic drugs in these models could happen in the near future.
3. THE POTENTIAL TO UTILIZE PERSONALIZED MEDICINE.
Some gastrointestinal diseases are genetic, like juvenile polyposis syndrome. We think that we could potentially use both a tissue-engineered colon and CRISPR/Cas9 technology (a tool that allows scientists to edit sections of the genome by changing parts of their DNA) to correct a patient’s genetic mutation and then reintroduce the proper tissue back into him. In theory, there should be no issues with transplant rejection because the immune system should recognize the patient’s own tissue. The potential is very exciting, but could still be another decade or two before we hone the technology in this way.
4. THE POTENTIAL TO TEST ABSORPTION OF OTHER DRUGS.
We think there is a potential for us to test all different types of drugs, not just ones related to gastrointestinal diseases. When patients take a drug orally, it passes through the inside of the intestines, which are 25 feet long. The drug can be absorbed into the bloodstream anywhere within this long tube, so utilizing the tissue-engineered colon could be useful for drug absorption studies. Because certain drugs may enter through the colon and not the small intestine, studying a colon model could tell us if oral delivery of a drug is a good option instead of using needles to inject into the blood directly.
5. THE POTENTIAL TO MODEL THE MICROBIOME.
The microbiome is made up of bacteria that live in the gut, and those bacteria are mostly concentrated in the colon. Modeling the microbiome in a tissue-engineered colon could allow us to study how the microbiome affects certain diseases. For instance, we could potentially study the role the microbiome plays in the obese versus non-obese.
Combining this discovery with our colleagues’ tissue-engineered intestinal research will allow us to gain a better understanding of how each of these regions of the gastrointestinal tract function separately and together. Because of the large prevalence of GI diseases in children, like colitis, colon cancer, irritable bowel syndrome and polyposis syndrome, this new research will open a gateway to other research projects considered undoable just a year ago.





