Alexis Shapiro’s story caught the attention of many people from around the country, including news outlets, generous individuals who wanted to help change the outcome, and those who were curious to learn more about the complex biological condition that caused her to gain excessive amounts of weight despite every attempt from her, her family, and her doctors to stop it.
While this one story has been told by many national news outlets, what hasn’t been covered in detail is how this condition known as hypothalamic obesity (HyOb for short) causes massive and rapid weight gain and how stomach surgery called gastric bypass may help people with this condition.
HyOb is a complex, biological condition which can result from the growth of a rare brain tumor called a craniopharyngioma. This type of tumor and/or the surgery to remove it damages the hypothalamus, which can have a dramatic effect on appetite and weight regulation. In fact, about 50% of patients with intracranial tumors like craniopharyngioma go on to develop HyOb.
The brain has the task of regulating an enormous number of processes every day, some that we are aware of (for instance, talking and walking) and some that we are not (body temperature, maintaining a normal weight). For weight regulation, a tiny part of the brain called the hypothalamus provides signals to the gut and other parts of the body, and gets back signals from the gut and from fat cells. They send signals back and forth, informing the other of hunger, fullness, and when to stop eating.
This process of proper communication about supply and demand between the brain and gut is about 99.8% accurate, allowing most (adults) to eat and burn almost the exact same number of calories every day and keep a reasonably constant weight. But for patients with HyOb, the communication between the brain and the gut goes haywire.
The hypothalamus controls many bodily functions that we consider automatic, including how many calories we take in per day and how many we burn. When the hypothalamus has been damaged, it no longer has the ability to regulate body weight, in part due to excess stimulation of insulin production.
Excess insulin increases appetite, causes irritability and weight gain regardless of strict dietary intake and exercise. Another important aspect of HyOb is the fact that the hypothalamus does not “hear” the signal that comes from the fat (a hormone called leptin) which is supposed to tell the hypothalamus to turn off “hunger.” Since the hypothalamus is resistant to the leptin signal, the person with HyOb continues to be hungry, continues to eat (a term called hyperphagia), continues to store the food eaten as fat, and never feels full.
This vicious cycle repeats every day as more and more weight is gained. The typical locations for safe storage of fat (for instance, beneath the skin) are eventually overwhelmed and then the body begins to store it in other places that are more harmful to health (in the muscles, liver, and around other important organs in the belly). With this excess fat being tucked into all of these important organs, they can’t do their jobs right and the net result is poor functioning and even inflammation in many of the body’s vital organs.
People with HyOb constantly feel like they’re starving and can gain upwards of 1-2 pounds per week even though they try to maintain calorie-restricted diets and exercise routines.
So what can be done for patients with hypothalamic obesity? Our Surgical Weight Loss Program for Teens and similar treatment programs at other hospitals have found that gastric bypass can be a successful measure for controlling hunger in patients with HyOb and for getting control of the weight gain. In addition to gastric bypass, we also consider a partial vagotomy (surgical removal of the vagus nerve). The vagus nerve is thought to transmit the powerful signals from the brain to the pancreas, which in the case of HyOb, results in excess insulin production. A vagotomony cuts the nerve and removes a portion of it, thereby interrupting these insulin production signals.
Together, bartiatric surgery and vagotomy alter the communication between the gut hormones, the autonomic nervous system, and the brain circuitry regulating hunger and energy balance. Interference with the vagus nerve signaling reduces communication from the central nervous system to the pancreas, which slows insulin production in response to meals.
We have found that patients undergoing these laparoscopic procedures have not only experienced weight loss, but also a reduction in other associated medical issues, such as reduced insulin and early reduction in leptin levels.
The results our patients have experienced are similar to the findings of a study that took place in Europe, in which I also participated. We reviewed 21 cases worldwide of patients undergoing bariatric surgery following surgical treatment for craniopharyngioma. This study was done to try to summarize the 12-month post-surgical outcomes for each of these patients that had been published. When the results were combined, average weight loss per person totaled 79 pounds 12 months after surgery.
But it’s important to keep in mind that bariatric surgery isn’t an option for everyone. In fact, it is only recommended in cases in which health is adversely affected and all other weight-loss measures have been attempted.
Patients with hypothalamic obesity fight many uphill battles associated with the disease. Not only are they trying to manage their uncontrollable weight gain, but they are often fighting the painful stigma, teasing, and ridicule that goes along with the disease.
They do not lack willpower, motivation, initiative, or discipline; in fact they have more drive and desire to lose weight and control their food intake than most people! Yet they face an overwhelming amount of obesity prejudice, based on the feeling that if they only stuck to their prescribed diets and recommended exercise routines, they could lose weight on their own. This can lead to isolation and regression from school, friends, and participating in activities that used to bring them joy.
We want patients to know that they are not alone and they are not to blame for their condition. Medical science tells us that hypothalamic obesity is a biological condition which causes miscommunication between the brain and the gut.
Because HyOb is so rare, we have started an online patient registry. It was established to increase awareness, facilitate future research, and improve treatment of this disorder. If you or someone you know has the disease, please pass the link along to them and share this post to help spread awareness.
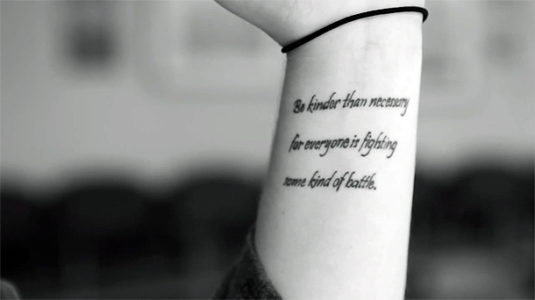
Editor’s note: In the picture at the top of the blog post, a teen who received gastric bypass surgery at Cincinnati Children’s has the following quote on her wrist,”Be kinder than necessary because everyone is fighting some kind of battle.”





[…] have published reviews and their own unique findings on this topic. Dr. Inge recently wrote a blog post explaining exactly how this procedure can potentially help counteract the miscommunication between […]