A few years ago, I met a family from Minnesota seeking an additional opinion about care for their teenage son, Bryce. He had autism as well as liver disease, which had recently worsened. He had developed hepatic encephalopathy, a condition seen in advanced liver disease that causes confusion, irritability, change in school performance, disorientation, and increased daytime sleepiness. It is typically an indication for liver transplant.
In Bryce’s case, two other hospitals his family had visited—the only transplant hospitals in Minnesota—declined to offer a liver transplant due to concerns he would not be able to manage the high level of care it required.
His family wasn’t willing to let that be a barrier so easily—and neither was I.
A PASSION FOR COLLABORATIVE CARE
One of the many reasons I came to Cincinnati Children’s 10 years ago was the family-centered care provided here. At that point in time, family-centered care was in its infancy, and Cincinnati Children’s was leading the way. I wanted to be a part of that.
Not only did I find the care here to be family-centered, but also multidisciplinary—where people from a wide variety of areas within the hospital work together to offer the best possible outcomes for patients. Both models of care are ones I embrace.
With the patient I mentioned above, from my team’s perspective in the Pediatric Liver Care Center, he was a good candidate for transplant. There were some behavioral concerns related to his autism, but his medical care was well managed, he was going to school, and he had enjoyed a good quality of life before he developed hepatic encephalopathy.
To address his behavioral concerns, we decided to form a team to address his needs. Before he arrived, I asked for input from a pediatric psychologist from Behavioral Medicine and Clinical Psychology who works closely with the liver transplant team. I also explained the situation to our Behavioral Safety Team and Adaptive Care Team and asked them to sit in on the initial evaluation and transplant team discussion, meetings they normally wouldn’t attend.
They were comfortable with the behaviors presented and noted that they were ones they commonly help patients with. They felt confident they could help throughout the process, both pre- and post-transplant. That, in turn, gave us the confidence that we could successfully move forward with a liver transplant.
PRACTICING BETTER MEDICINE
In addition to the help we received from Behavioral Medicine and Clinical Psychology and the Behavioral Safety and Adaptive Care Teams, we worked with many others throughout Bryce’s time with us: Nephrology, Psychiatry, Endocrinology, Genetics, Critical Care, Surgery, Child Life, Nursing, and so many others. It was a big list, and every person who engaged in Bryce’s care contributed to his success. Relying on the expertise of colleagues within our medical center, we were able to challenge perceived medical and behavioral barriers and support both him and his family through the liver transplant process. This is the benefit of multidisciplinary care.
I feel strongly that we can practice better medicine when people from different fields meet, examine what’s going on, and come up with a plan together. We see the benefits of this in so many places: when creating care plans, preparing for surgery, during a patient’s recovery and after discharge.
ADVOCATING FOR CHILDREN
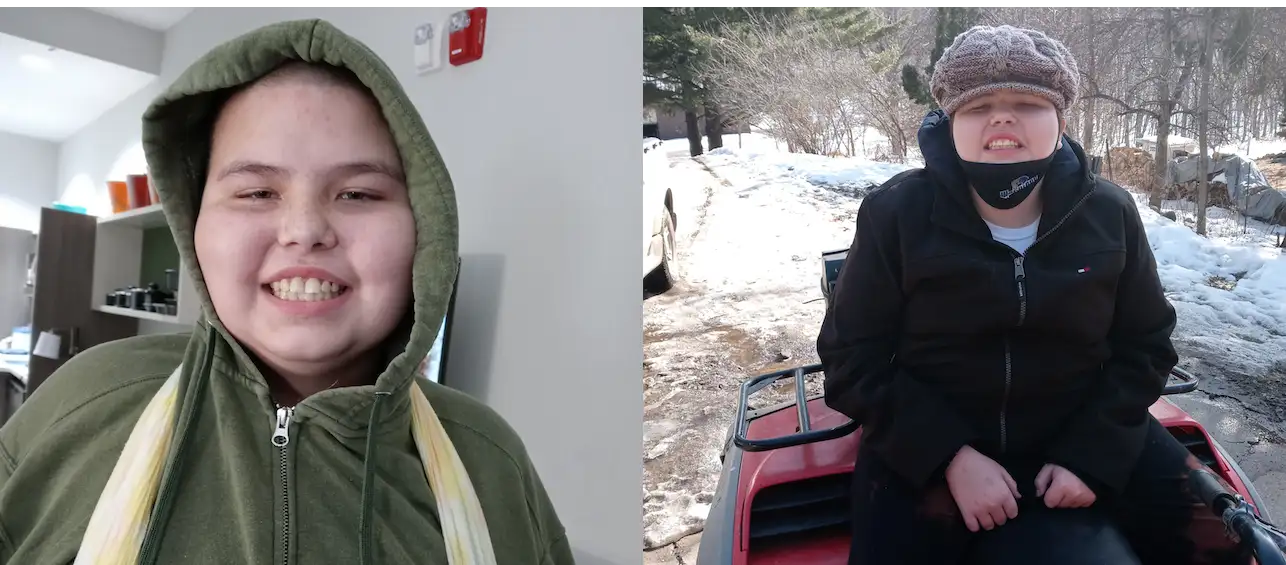
Bryce went on to have his liver transplant, and I am thrilled to say he is now doing so well. I receive pictures of him from his mom: back at home in Minnesota working on his family’s farm, riding tractors, and doing the things he had done before he developed complications of liver disease. He’s gotten his quality of life back.
His mom, Nikki, was a big part of the reason why he’s in that place. She was a huge advocate for him and the care he needed. She could have stopped when that first hospital told her he wasn’t a good candidate for a transplant. But she didn’t.
We hold our patient families in high regard here. They know their child best, and that’s an important factor when planning medical care. We like to include parents as part of the care team, knowing that their input can be just as crucial as a doctor’s. From a physician’s point of view, it’s very rewarding to partner with parents and patients in their care, to make decisions together, recognizing that things don’t happen to patients in a vacuum.
This story is just one of many examples of collaborative care that I could bring up to show why I’m proud to be here at Cincinnati Children’s. I wholeheartedly believe in working together with others so we can come up with the best possible care plans for our patients. It’s the kind of care I would want for my own children, and it’s the kind of care I’m proud to provide to my patients.
Editor’s Note: Bryce’s mom, Nikki, wasn’t satisfied with Bryce being refused treatment due to his disabilities. A true advocate, Nikki pushed for statewide change and succeeded. Says Nikki, “Because Cincinnati Children’s gave Bryce a chance, a law in Minnesota has since been put in place based off of Bryce’s story for fair treatment for transplant for people with disabilities. The law and Bryce’s story are also moving forward federally. So the treatment Bryce received from Cincinnati Children’s did not only save his life but will affect millions in the future.”






I am extremely grateful for the amazing people that helped Bryce and my daughter, his mom Nikki. I don’t know what we all would have done without the help from the doctor’s and staff at Cincinnati’s children’s hospital. Again thank you all so much!!!!!