I was diagnosed with congenital hip dysplasia immediately after birth.
My clicky hips were treated with the 1980s version of the Pavlik harness, triple cloth diapers. As a child, I was a masterful toe-walker and contortionist that enjoyed w-sitting, doing the splits and dancing on my toes. These “skills” along with my keen ability to push through pain, served me well throughout my championship Irish dancing career and into my young adult hobby, long distance running.
Pushing Through The Hip Pain
I never sought out a diagnosis to explain lower extremity, hip and back pain in adulthood. I was scared to know what was wrong and didn’t want someone to tell me to stop sports. So I ignored the symptoms and rationalized that high impact sports and “getting older” were supposed to hurt.
I first met Dr. Whitlock in March of 2015 to screen my infant daughter for hip dysplasia. Coming into this world she had three of the five hip dysplasia risk factors – female, a breech presentation and positive family history including her aunt, multiple great aunts and me. Dr. Whitlock ordered ultrasounds, x-rays and performed hip exams at several points during her first year.
Fortunately, she never required treatment. During one of those visits, I mentioned that my hips hurt and that they were impacting my ability to fulfill my role as full-time working mother and wife. My normal was taking daily NSAIDs, sitting on the sidelines and sleeping with ice packs to manage my hip, low back and nerve pain. He explained that hip pain at my age was not normal and encouraged me to schedule an appointment because “the longer you wait, the fewer options you will have.”
A Re-Diagnosis of Bilateral Hip Dysplasia
After I got over the phenomenon of being an adult patient in a children’s hospital, I heeded his advice. At the age of 32, he re-diagnosed me with bilateral hip dysplasia. Many adults with hip dysplasia see multiple doctors and wait years in pain for an accurate diagnosis.
I was lucky to have a daughter that lead me directly to the right doctor at the right time. A doctor that knew the source of my pain and could fix it. She was breech for a reason! After six weeks of physical therapy which exacerbated the symptoms, he recommended that I consider surgical treatment.
Periacetabular Osteotomy to Reduce Pain and Joint Deterioration
A periacetabular osteotomy (PAO) was recommended as a treatment option to address the structural abnormality. A PAO is a big surgery with a significant recovery time of six months to a year. Multiple bones in the pelvis are fractured to allow the shallow socket to be detached and repositioned to better cover the femoral head.
It does not cure dysplasia. The intent of the surgery is to provide better stability to the joint, thereby, slowing the rate of joint deterioration and reducing pain. After I received a second opinion, I decided to proceed with a bilateral PAO at Cincinnati Children’s to save my hips.
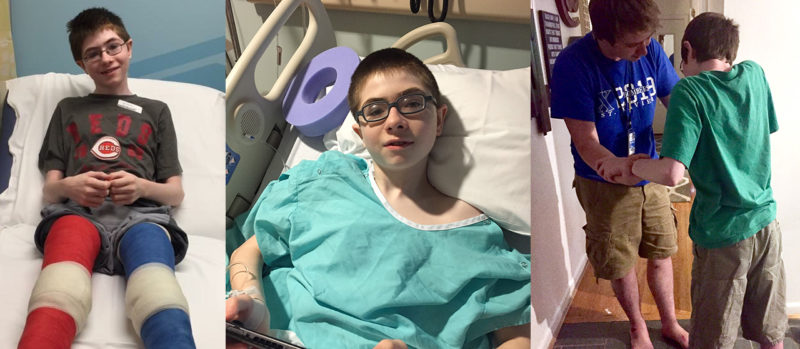
The surgeries were in November 2015 (left) and May 2016 (right). They were six months apart to allow for ambulation and recovery. I’m going to be transparent. The surgeries were painful and the recoveries were grueling. They were the hardest thing I’ve done in my life — and I’ve had two kids.
I was on crutches for 6-10 weeks and in physical therapy for over a year. The care from Dr. Whitlock and the rest of the Hip Preservation team was phenomenal. Their knowledge and support gave me the confidence and hope to persevere through a difficult year of surgery and rehab. I am now two years post op from my first PAO. Drawing from my personal experience, below is the advice that I can offer to future and current PAO warriors:
Advice for Other Adults Facing a Periacetabular Osteotomy
1. Set Realistic Expectations
Get on the same page with your doctor. Life is all about expectations. If they’re unreasonable, you’re setting yourself up for disappointment. A realistic outcome for me was to get through my day without debilitating pain. NOT achieving marathon personal records.
2. Be Kind to and Patient with Yourself
Things will get worse before they get better and they will get better. This process is grueling and recovery is not linear. It helped me to keep a list of my accomplishments: putting my shoes on, sleeping on my stomach, walking without assistance, etc. On tough days, I could read it and be reminded that I was moving in the right direction.
3. Listen to Your Body
Don’t push through pain and, if you’re tired, rest. Your recovery will be impacted if you don’t respect your body’s signals. Being a doer and a pusher, I had to learn this lesson the hard way. I gave myself a nasty case of hip flexor tendonitis and my incision took ages to heal. Don’t be like me, downshift before you are forced to slow down.
4. PT is the Key to Get the Outcome You Desire
Open communication and compliance are essential to success. If you choose to have this surgery, you must commit to make PT a priority for at least 6 months. It’s hard to find a PT with PAO experience, so seek one out that is open to learning and ongoing communication. I was in the gym five days a week. I studied hip and spine anatomy in my spare time to become more in tune with my body. This helped me clearly communicate my areas of weakness and pain. I’m confident this extra homework helped my PT tailor a plan to effectively address years muscle dysfunction.
5. Rally and Accept Support From Friends and Family
You will need help! I would not have been able to go through with these surgeries without the assistance of family and friends. Everyone in my family has pitched in, from watching my kids to giving me blood thinner injections, to cooking meals and everything between. Additionally, I found so much value in having a PAO buddy. I was blessed to find a local gal with hip dysplasia through a mutual friend. We had our bilateral PAOs done around the same time. It was so important for us to have another person in our life that GOT IT. She is my silver lining.
Throughout diagnosis, treatment and recovery, I have felt supported, listened to and cared for by the Hip Preservation team. They have gone above and beyond to get me well and continue to do so. My left-side is much improved and my complex right side is a work in progress. I’m not where I want to be yet, but I’m confident that I will have an excellent outcome because my care team will not give up until I’ve gotten it.
To learn more about our Hip Preservation Program, please call 513-636-2371 or submit an online form for more information.





Are children treated for hip dysplasia at increased risk for adult hip dysplasia? I feel like the connection is implied in the article but never stated. My friend’s daughter had surgical intervention for hip dysplasia as a toddler in Australia. I thought once the surgery was successful, that was the end. But based on the article, my thoughts are incorrect. What is the percentage of recurrence in adults?
Hi Jess,
Thanks for your question! I reached out to Dr. Whitlock for his perspective. Here’s what he had to say: Although the majority of children successfully treated for hip dysplasia go on to need no further intervention and lead similar lives to children without dysplasia, treatment as a child does not necessarily mean that the child will not go on to possess or develop symptomatic dysplasia as an adolescent or adult. Treatment requires tailored, long-term followup that is individualized to that patient’s overall diagnosis and treatment.
Shannon, please visit http://www.EDSawareness.com The description of your childhood is typical for EDS, as is hip dysplasia. I’m glad you are doing amazing!! I have a few adult EDS clients contemplating PAO surgery. I’m definitely going to share your story!!
Dr Whitlock is an amazing surgeon. I have several kids in my EDS support group that see him and have had some major surgeries without complications. We love him!!
Powerful testimony, Shannon. Thanks for sharing your story!
I have a 4 yr old daughter who was just diagnosed with hip dysplasia in both her hips. 2 different doctors recommend surgery. I’m torn. I don’t want her to go through the surgeries but I also don’t want her to go through what I am going through. I was diagnosed with degenerative joint disease in my teens. What advice do you have for me?
Hi Autumn,
I recommend reaching out to our Hip Preservation Center directly at 513-636-4785. Or you can fill out an online form for more information here: https://www.cincinnatichildrens.org/service/h/hip-preservation-program/contact/online-form They will be better able to answer your questions or point you in the right direction.
Thank you so much for sharing your story. I am 44 and have just been diagnosed with hip dysplasia. I had an arthroscopic surgery to repair my very shredded labrum, and the surgeon also removed some bone spurs. My healing has been as expected according to my surgeon. I am 8 weeks post surgery and experiencing daily pain, tendonitis, and I cannot walk without a cane. I really expected things to go much differently and heal quickly. The question I have is, with this condition, is it realistic for me to safely return to my very active lifestyle and hard labor jobs? Currently I am not able to work and it’s starting to look like planning to return might be a very bad idea. I am expected to stand and lift , bend and work on slippery floors.
Hi Allicat,
Thanks for your question! I reached out to Dr. Whitlock. Here’s what he had to say:
Each patient’s recovery is unique. Depending on the severity of disease, hip patients can usually expect to return to full activities of daily living within 3-6 months. Return to impact sports and other recreational activities may take longer and they may not return to their original level prior to experiencing pain. If they have symptomatic dysplasia, an arthroscopic surgery may help with the symptoms but will probably have little effect on treating the underlying condition. Arthroscopy may have been the best choice for your hip, depending on your stage of joint degeneration.
Hope this helps!
Hi there! I had a right reverse PAO 13 weeks ago and I think I’m experiencing hip flexor tendonitis. I have horrible pain in the front of my hip and it’s exacerbated by doing anything which causes me to use my hip flexors. What worked for you to ease the pain if you don’t mind me asking? I’m supposed to return to work in a week and a half and am very nervous. Thank you in advance!
Hi Lauren! I’m so sorry. I just saw your post. Feel free to email me at shanofshaw@gmail.com. I’m more than willing to chat!
I had this surgery at age 48. I still have numbness on my thigh. But I can walk without pain. I have to stretch daily or my hip flexor tighten up too much. I feel the PT should have been longer. I returned to PT last year cause of pain in my lower back and buttocks.