What we know about medications and how they affect the kidneys has evolved over the last decade.
More awareness is needed around this new knowledge because what we’ve learned about nephrotoxic medications is that they can lead to poor outcomes – and in many cases, the situation is preventable.
Nephrotoxic medications are defined as those that cause harm to the kidneys. Many prescription 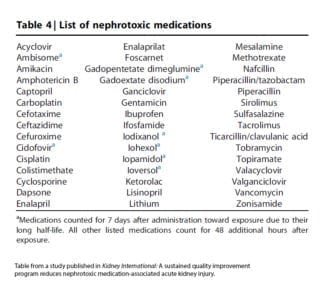 medications used for complex or chronic conditions like cancer, congenital heart disease and cystic fibrosis can be nephrotoxic, but even some over the counter medications like ibuprofen and naproxen can cause damage as well.
medications used for complex or chronic conditions like cancer, congenital heart disease and cystic fibrosis can be nephrotoxic, but even some over the counter medications like ibuprofen and naproxen can cause damage as well.
For reference, I have included a list of nephrotoxic medications to the right but please keep in mind that many of them are life-saving and I’m not suggesting that your child should stop taking them. Rather, I recommend for parents to be aware of the medications that are potentially harmful to the kidneys and to have a conversation with their child’s care provider about how much is necessary to treat the condition and if there are any potential alternatives.
Here are some of the most important things for parents to be aware of related to nephrotoxic medications:
- Nephrotoxic medications can cause an acute kidney injury (AKI), which is an abrupt loss of kidney function. The kidneys are responsible for filtering all of the waste products from the food that we eat out of our blood and maintain fluid balance so that we don’t dehydrate or get fluid overload.
- Having an AKI can lead to poor outcomes. What we know from analyzing data about our patients and conducting research here is that when children have an AKI, depending upon their situation and reason from coming to our medical center, they have poor outcomes as a result, such as the development of chronic kidney damage, chronic kidney disease, or a greater chance for mortality if they are critically ill.
- Kids who are hospitalized and/or have a complex condition are at high risk for AKI. Because modern medicine has evolved so well, therapies for some pediatric diseases like congenital heart disease, cancer, and cystic fibrosis have allowed patients to survive and in some cases, thrive. However, many of the medications that these patients are on are so powerful and nephrotoxic that they treat the original problem but they cause irreversible damage to the kidneys.
- If AKI is caught early, it can be mitigated. The good news is that if elevated levels of a simple blood test called creatinine is detected early, AKI can be mitigated. The difficult part is that in most cases, acute kidney injury does not have any visible side effects.
So how do families watch out for it? If your child has been hospitalized or is undergoing treatment for conditions like congenital heart disease, cancer or cystic fibrosis, ask your child’s doctor questions like “Is my child at risk for AKI?” or “Are you assessing my child for AKI?” or “How will you be checking for AKI?” - AKI can be detected with a simple blood and/or urine test. We have determined through research that the threshold for AKI is much lower than originally thought. So it’s important for patients who may be at high risk for AKI to have their levels checked earlier. Currently at Cincinnati Children’s, we’ve formalized that process by implementing a program called NINJA, which stands for Nephrotoxic Injury Negated by Just-in-time Action.
Here’s a short explanation of what this program does for children treated at our medical center: children who are receiving three or more nephrotoxic medications at once – or a particular antibiotic that is known to be nephrotoxic – for more than three days, they will receive a daily check of their kidney function through that simple blood test, creatinine.Through this formalized process, we’ve learned that there is an epidemic of acute kidney injury from nephrotoxic medications. One in four kids who received these nephrotoxic medications (in one of those two ways) developed an AKI. - The NINJA program (or even considering the nephrotoxicity of medications) reduces nephrotoxic exposure and AKI. After we implemented this program to monitor what nephrotoxic medications our patients were receiving and sharing that data with their main care providers within the hospital, they used that information to make better decisions about which medications to use to treat their patients’ conditions and consider how long they actually needed to be on them.
After the first few years of implementation, we saw a 60% decrease in the incidence of AKI. And even if your child’s hospital isn’t currently using this program – it’s been implemented in 13 children’s hospitals so far — you can ask your child’s doctor to continually monitor your child’s kidney function. - Everyone who takes a nephrotoxic medication is at risk. Thinking about AKI is important for everyone, not just hospitalized kids or kids with a complex or chronic condition. There are certain over-the-counter medications that are particularly toxic to the kidneys – even at the recommended doses. Ibuprofen and naproxen are two examples.
Student athletes are of particular concern here because they take ibuprofen for muscle pain and they are often dehydrated at the same time (a bad combo for the kidneys). It’s paramount for your children to be hydrated when they’re taking a nephrotoxic medication and if they’re requiring it for more than a day or two, you should make sure that your child’s doctor assesses their kidney function to make sure that they’re okay.
The bottom line is that nephrotoxic medications have helped children survive and thrive beyond the original condition for which they were either treated or hospitalized – and they shouldn’t stop taking them. However, through our most recent research and better understanding of nephrotoxic medications over the last 10 years or so, it is our determination that children should only take the ones that they need and only for the length of time that they need them in order to mitigate the risk of an acute kidney injury.






I feel that any drugs taken, will eventually affect the liver and the kidneys, along with other organs, as well, if taken for long periods of time. Sometimes even for a few days. I would love to know what CF drugs might contribute to AKI, as our son has CF. I also know that he watches and is well aware of the affects that some of these drugs have on the body. There are some that are taken, that need to be, in order for CF patients to be able to stay as healthy as possible. It’s definately a double edged sword, so to speak. Thanks